A 3-year-old's epilepsy care is uncertain due to UnitedHealth-Fairview dispute
Published in Business News
CHANHASSEN, Minnesota — Keeping Parker McEnaney smiling has required well over a dozen expensive drugs, a medevac flight to California and the expertise of just about every specialty team at M Health Fairview Masonic Children’s Hospital in Minneapolis.
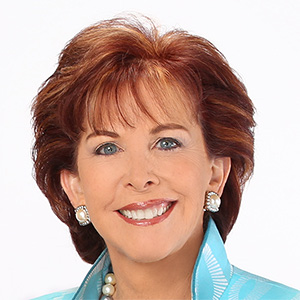
A cord snaking into the 3-year-old’s grippy sock connects to a device reading her pulse, which her parents use to detect when Parker is seizing. This has occurred up to five times per day for most of Parker’s life, each time feeling like “absolute chaos,” said her mother, Anna McEnaney.
Parker’s parents are part of her care team, and their work is about to get more complicated because of a thorny contract impasse between their insurance company, UnitedHealthcare, and M Health Fairview.
“It’s really scary to think that we’re gonna lose our home — because Masonic is our home — that we’re gonna lose our safety net. That we’re gonna lose our team that understands us, that advocates for her,” Anna McEnaney said, sitting with Parker as she pulled her rosy cheeks into a grin.
Fairview Health Services says it might leave UnitedHealthcare’s commercial network next year in a dispute that would prevent about 125,000 people, including Parker’s family, from scheduling appointments with Fairview doctors beginning in January. The change applies to people who receive insurance through work.
The health system argues that UnitedHealthcare’s payment rates have fallen short. The insurer counters that Fairview is demanding a 23% price hike over three years that would spike costs for employers. Contract disputes between insurers and health care providers have been growing in recent years, usually resolving before any network disruption takes place. For patients, though, they fuel uncertainty.
“Please, dear God, resolve the dispute,” McEnaney said.
Parker sat cozily in floral pajama pants and a purple long-sleeve shirt last week. Anna McEnaney said Parker’s 7-year-old sister adores her like a baby doll. Parker loves watching Bluey and sticking her hands on the dark fur of Malcolm, the family’s “gentle giant” dog, the mother said.
“With the conditions that Parker has, every day with her is a blessing,” Anna McEnaney said. “Epilepsy is a beast that I wouldn’t wish on anybody.”
After arriving home from a typical birth in December 2021, Parker was trying so hard to breathe that her stomach caved inward with each huff, Anna McEnaney said. The parents took her back to M Health Fairview Southdale Hospital, where she experienced her first seizure when she was 72 hours old.
Parker then transferred to Masonic to stay in the neonatal intensive care unit for six weeks, and her family fell in love with the children’s hospital, said Joe McEnaney, her father.
Doctors diagnosed Parker with several conditions: cerebral palsy, cortical visual impairment preventing her brain from processing what she sees, and a severe form of epilepsy called Lennox-Gastaut syndrome. Parker’s condition is so medically complex, Anna said, that the smallest of tweaks to her treatment “could just send her into outer space.”
When a seizure occurs, Parker’s parents must figure out whether to administer supplemental oxygen or rescue medication. They debate if they will call an ambulance or phone the hospital first. Her two siblings have watched her “turn purple,” Anna McEnaney said.
Parker’s future is uncertain, Anna McEnaney said, so the family takes things day by day.
“We’re not sure how long we’ll have with her,” the mother said. “But I know that if it’s with Masonic, we’ll be good and we’ll be safe.” When Parker visits the children’s hospital in Minneapolis, the staff always seems ready, Anna McEnaney said.
More than 20 specialty teams there have helped her try out more than a dozen medications and undergo multiple surgeries, Anna McEnaney said. In more than 400 appointments, the staff encouraged the parents to pursue second and third opinions and spoke honestly about Parker’s future.
When Parker headed to the emergency room after a urinary tract infection triggered dozens of seizures in less than two days in August, the staff recognized her and quickly put her mother on the phone with a neurologist.
The staff previously wrote a letter to UnitedHealthcare, explaining why a pricey medevac flight to California was necessary for Parker to undergo a corpus callosotomy procedure severing the fibers connecting her brain’s halves, her mother said. This would help doctors explore the cause of her epilepsy.
A medication Parker takes would have cost more than $125,000 per month if not for the family’s insurance coverage, Anna McEnaney said. UnitedHealth Group, based in Eden Prairie, has covered a lot of expenses, leaving the mother “forever grateful.”
Parker is responding well to a new medication and hasn’t had a seizure in 10 weeks. But now, the medical system and insurer are not getting along.
When a Fairview letter arrived that said the McEnaneys might have to find new providers, the mother “said a lot of choice words,” she joked.
“And then I cried a lot.”
Joe McEnaney said he wouldn’t even know where to start in reestablishing care with a dozen or so specialty programs.
The parents are trying to book Parker’s appointments before the end of the year. Her secondary Medicaid insurance could provide more time, but amid federal cuts, much is still uncertain.
A UnitedHealthcare spokesman said in an email that the insurer is working to assist the family. University of Minnesota physicians will remain in-network for patients regardless of whether Fairview exits the network, he added.
“Our number one priority is providing people continued, uninterrupted access to the care they need,” the spokesman said. He said other children’s hospitals such as Gillette Children’s and Children’s Minnesota remain in-network.
Patients receiving treatment for serious or complex conditions such as cancer or pregnancy at a Fairview hospital or from one of its physicians may be eligible for “continuity of care,” he said. This provides continued in-network benefits for a period of time after a provider leaves the network. Patients may call the number on their health plan ID card if they have questions about continuity of care, he added.
Dr. Jaya Kumar, M Health Fairview’s chief medical officer, said in a statement that Fairview is working urgently to reach an agreement with UnitedHealthcare.
Kumar said the insurer’s “administrative barriers, denials, and below-market rates create challenges that directly affect patients and our ability to care for them. That’s why we are asking for fair, sustainable terms that align with what nonprofit insurers provide.”
“We continue negotiating in good faith because no one should have to worry about insurance when they’re focused on getting well,” she said.
Anna McEnaney said she understands both the insurer and medical system must make money. “But we’re just caught in the middle of them going back and forth.”
“Starting fresh is —” Anna paused. “I don’t know how we would ever do that. These are people who’ve grown up with her.”
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.














Comments