Lisa Jarvis: What if the COVID vaccine could save cancer patients too?
Published in Op Eds
A stunning new study offers early evidence that COVID-19 vaccines might have a secret superpower: a precisely timed mRNA shot could help many cancer patients live longer.
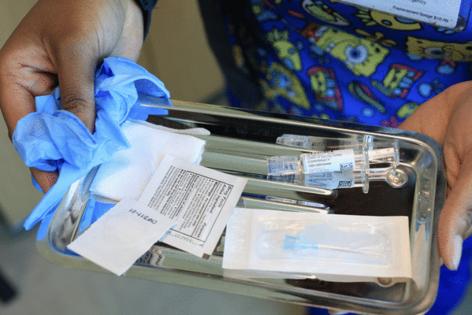
The work still requires validation, but the strength of the signal in the study — which analyzed differences in outcomes between cancer patients who did and did not receive mRNA vaccinations during the pandemic — should be sufficient motivation to direct resources toward quickly obtaining a definitive answer. COVID vaccines are inexpensive, widely distributed and easily accessible at most local pharmacies, such as CVS. If the findings hold true, they could offer a simple and cost-effective way to improve patients’ lives.
Yet the current administration’s dismissive stance toward mRNA science, particularly COVID vaccines, could impede that effort. This new research should push the nation’s health leaders to reconsider the enormous potential of this Nobel Prize-winning technology.
The study, published earlier this month in Nature, originated from a curious observation made by Adam Grippin, a radiation oncologist at the University of Texas MD Anderson Cancer Center, while working on his PhD thesis at the University of Florida. He was helping to develop personalized mRNA vaccines for people with brain cancer, designed to train the immune system to recognize specific markers on a patient’s tumor and launch an attack. But when testing the bespoke shots in animals, Grippin noticed that even the placebo shots — which contained mRNA entirely unrelated to the cancer — also activated the immune system to kill tumors.
“Since then, I have spent pretty much every day thinking about the results,” Grippin told me. The implication was that there could be an easily accessible, off-the-shelf shot capable of stimulating the immune system to fight cancer.
Grippin and his colleagues analyzed medical records from more than 1,000 patients with advanced lung and skin cancers who had undergone treatment with a type of immunotherapy called checkpoint inhibitors. People who received an mRNA-based COVID vaccine — it didn’t matter whether it was Pfizer or Moderna’s — up to 100 days before starting immunotherapy were twice as likely to be alive as those who either didn’t receive the vaccine or got it outside that time window.
The researchers also looked at whether the flu and pneumonia shots produced a similar effect (they didn’t) and whether patients who received a COVID vaccine in tandem with other cancer treatments benefited (they did not).
To understand what makes the mRNA shots special, the researchers examined blood and tissue samples and found that the COVID shots appeared to activate the innate immune system — a fundamental, early-warning defense mechanism that alerts other parts of the immune system to prepare for an attack.
That something as simple as a COVID vaccine might improve survival in cancer patients receiving standard immunotherapy has taken oncologists by surprise — in a good way. “My initial reaction was surprise and maybe disbelief,” says Ryan Sullivan, director of the Melanoma Center at Massachusetts General Hospital. Scientists are natural skeptics, and his first instinct was to look for flaws. Yet after carefully reviewing the paper, he concluded that the researchers had done extensive work to explain their findings and account for potential confounding factors. “The data are really good,” Sullivan says. He added that the sheer number of patients included in the retrospective study made the results especially compelling.
Of course, all of this needs to be confirmed in a randomized, placebo-controlled study, and the MD Anderson doctors are already planning one. Ideally, clinical trials will be paired with basic research to help scientists answer the many questions this discovery has raised.
For example, the benefit only appeared when people received their COVID shot within a specific window before starting immunotherapy. Determining the optimal timing to maximize that benefit would be crucial if this were to become part of standard treatment guidelines. After all, a doctor might be speaking with a patient who has newly diagnosed advanced cancer and feels an urgency to start treatment — should they wait a few days after vaccination, or would a few months be better?
Cancer immunotherapy is used to treat many common cancers, including breast, colon and bladder, and doctors want to know if the COVID shot might also help extend survival for those patients. Physicians at MD Anderson have conducted comprehensive reviews of every patient receiving immunotherapy at their facilities since 2018 and have a paper under review that is expected to provide an early answer soon.
Researchers also want to know whether the effect, if validated, can be improved upon. The mRNA in COVID vaccines carries instructions for making the coronavirus’ spike protein, but what if a vaccine instead delivered instructions for a protein that could more precisely stimulate that innate immune response?
All of these questions deserve urgent exploration. Unfortunately, the discovery comes at a particularly difficult moment for mRNA vaccines. Health Secretary Robert F. Kennedy Jr., a notorious source of vaccine misinformation during the pandemic, is now in a position of authority over the nation’s research agenda and health policy. He has been steadily undermining support for COVID vaccines by unilaterally narrowing the Centers for Disease Control and Prevention’s recommendations and terminating funding for nearly two dozen mRNA vaccine-related grants.
Philanthropy and Big Pharma will likely step in to help fund clinical trials. But the consensus among academics is that obtaining government funding for mRNA research will be extremely difficult — if not impossible — for many projects.
The potential to help cancer patients is profound. The simplicity of the idea — that someone about to start immunotherapy could simply pop into their local pharmacy for an inexpensive shot that might prolong their life — should be enough to inspire everyone to put aside politics and invest in pursuing this promising finding.
______
This column reflects the personal views of the author and does not necessarily reflect the opinion of the editorial board or Bloomberg LP and its owners.
Lisa Jarvis is a Bloomberg Opinion columnist covering biotech, health care and the pharmaceutical industry. Previously, she was executive editor of Chemical & Engineering News.
_____
©2025 Bloomberg L.P. Visit bloomberg.com/opinion. Distributed by Tribune Content Agency, LLC.


















































Comments